Health
The Immortal Henrietta Lacks: Cells Of Deceased Black Woman Advance Medical Cures For 71 Years
BLACK HISTORY MONTY 2022-Week One
The Immortal Henrietta Lacks: Cells Of Deceased Black Woman Advance Medical Cures For 71 Years
By Leonard E. Colvin
Chief Reporter
New Journal and Guide
The theme for the 2022 observance of Black History Month (BHM) is “Black Health and Wellness.” It will address “How Black people have suffered a health legacy of indifference and disparity.”
Also, it will address how Blacks have overcome institutional biases and made great contributions to science and healthcare practices for all.
During slavery, except for the most productive ones, little concern was devoted to healthcare for Black men and women even after the civil war. But Blacks made their way to the profession.
Born in 1762 as a slave, James Durham is considered the first Black person to work as a doctor in America but he was not degreed in Durham, North Carolina.
Born in 1813, Dr. James McCune Smith was the first Black doctor to practice with a medical degree in the U.S. He earned his degree in Glasgow, Scotland, as he could not earn a degree in the U.S.
Dr. Rebecca Crumpler, born in 1831, was the first Black woman to earn a medical degree in the U.S. She practiced in Richmond, Virginia with the Freedmen’s Bureau.
Dr. Daniel Williams performed the nation’s first open-heart surgery and he owned Provident Hospital, the first interracial, Black-owned hospital which opened in 1893.
Dr. Charles Drew born in Washington, D.C. in 1906 was a surgeon and medical researcher in the field of blood transfusions, developing improved techniques for blood storage. He applied his expert knowledge to developing large-scale blood banks early in World War II, saving thousands of wounded soldiers.
Ironically, he bled to death after he suffered injuries in a car accident and reportedly was denied or delayed treatment at nearby White facilities.
The library of stories detailing African Americans’ advancement in medicine despite abuses, brutal racism, and exploitation is huge. But the story of Henrietta Lacks is a critical volume in that legacy of major healthcare contributions by Blacks.
The Amazing HeLa Cells
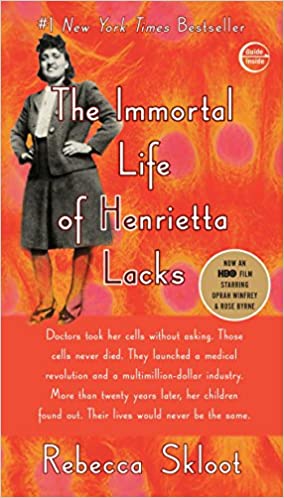
The story of Henrietta Lacks came to the public’s attention in a ground-breaking book, The Immortal Life of Henrietta Lacks by Rebecca Skloot, a reporter, in 2010.
Born Loretta Pleasant in 1920, in Roanoke, Virginia, Lacks, nicknamed Hennie, was a petite and charming woman. At age 21, she married David Lacks and the couple settled near Dundalk, Maryland, in Baltimore County. They had four children, the last in 1950 at Johns Hopkins Hospital
In 1951, Lacks was diagnosed with cervical cancer. Four months later, she died in a bed in the “Colored Ward” at Johns Hopkins Hospital in Baltimore.
Working down the hall at the hospital were Margaret and George Gey.
Gey was a researcher who had been attempting to grow human cells in his lab for decades, and before Lacks died, some of her cells were harvested and given to the Geys.
This unsolicited act would have a lasting and far-reaching impact on medical treatment and research until this very day.
Lack’s cells were discovered to have the miraculous ability to divide and replicate indefinitely outside the body. Unlike normal human cells which can reproduce themselves outside the body around 50 times before stopping, Lacks’ cells kept reproducing themselves indefinitely.
Called the HeLa Cells, 71 years later, Lack’s cells are still reproducing themselves. Scientists all over the world have used her cells to pursue and secure medical breakthroughs.
The HeLa Cells, as they are called, were used for the first polio vaccine. If you go to the online Library of the National Institute of health, and type in “Uses for HeLa Cells” you will see a patch of some 117,090 results.
They have been used for over 75,000 plus studies. Soumya Swaminathan, the chief scientist at the World Health Organization (W.H.O.)., said about 50 million metric tons of the HeLa Cells have been used by researchers and scientists around the world.
“This is just enormous when you think about it,” Dr. Swaminathan said. “I cannot think of any other single cell line or lab re-agent that’s been used to this extent and has resulted in so many advances.”
HeLa Cells have been reproduced billions of times, and used in research for Parkinson’s Disease, leukemia, and the flu.
They contributed to pave the way for the HPV vaccine, medications used to help patients with H.I.V. and AIDS.
Many of those diseases impact African Americans disproportionately at higher levels, including the disparities in the impact of COVID-19.
HeLa Cells were used for in-vitro fertilization which was the centerpiece of research at the Jones Institute in Norfolk, Virginia, which produced the first test-tube baby in 1981.
Howard Wilbur Jones, Jr., an American gynecological surgeon and in vitro fertilization (IVF) specialist, joined the faculty at Johns Hopkins in 1940. It was he who diagnosed, and initially treated Henrietta Lacks during an examination in 1951.
On February 8, 1951, Jones, according to his bio, took a biopsy of Lack’s cervical tumor and sent samples to his laboratory colleagues, thus beginning the evolution of the HeLa Cells which survived outside the human body.
The Joneses moved to Norfolk in 1979 and created an in vitro fertilization (IVF) program at the Eastern Virginia Medical School (EVMS) that resulted in the 1981 birth of Elizabeth Jordan Carr, the first test tube baby. He and his wife were affiliated with the Eastern Virginia Medical School (EVMS) until he died in 2015.
Today, two years into the COVID-19 Pandemic, and most recently for studying the effects of SARS-CoV replication in the human body, HeLa Cells have been used.
Initially during the research to fight the COVID-19 and its variants, cells claimed from elective abortions were used. But leaders of the Catholic Church in North America and other anti-abortion groups believed using those cells was unethical.
So the groups managed to sway the US Food and Drug Administration to instead provide incentives for Covid-19 vaccines that do not use fetal cell lines, including HeLa Cells.
Last year, 70 years after Henrietta Lacks died and was buried in an unmarked grave, the World Health Organization honored the contributions she unknowingly made to science and medicine.
During a ceremony in Geneva, Dr. Tedros Adhanom Ghebreyesus, the director-general of the W.H.O., presented the Director-General Award to Lacks’ son Lawrence Lacks, who was 16 when his mother died on Oct. 4, 1951.
Victoria Baptiste, Lack’s great-granddaughter, said the family was “humbled” by the presentation and the acknowledgment of the legacy of “a Black woman from the tobacco fields of Clover, Virginia.”
The image of Lacks, who would be 100 now, in the form of a statue was unveiled last year at the University of Bristol. But the issue of medical exploitation and racism color the entire legacy of Henrietta Lacks’ contributions.
While the nation’s biomedical firms have made billions of dollars on the outcomes of their research, the descendant of Heneritta Lacks have not reaped any financial benefits from their work which has saved the lives and health of millions.
They did not even know until 1973 that the cells were being used, at which time scientists called them for blood samples so they could study their genes.
But things may soon change for the heirs of Henrietta Lacks.
Last October Civil Rights Attorney Benjamin Crump, known nationally for representing the victims of police violence, filed a suit on behalf of Henrietta Lacks’ estate.
“Why is it that everybody else can benefit because of her cells, yet her family has not received one red penny?” Crump said during a story produced by NPR shortly after he filed.
The target of the suit is Thermo Fisher Scientific, which sells a commercial line of HeLa tissue.
The suit accuses the biotech company near Boston of unjust enrichment because the company continued to profit from HeLa cells, even after learning that Henrietta Lacks never gave her permission for them to be taken or to be used in that way.
“So I have to tell this story,” said Ron Lacks, Henrietta Lacks’ son.
“I have to take back control of Henrietta’s legacy. This is not right.”
Glenn Cohen teaches law and bioethics at Harvard and says what happened to Lacks wasn’t unusual.
Cohen, interviewed for the same NPR story, said the suit may be hard to convince the courts.
“There’s a legal matter at the time in which the tissue was taken. It was not the ethical rules of the day to require informed consent,” he said.
“Another problem is precedent. People who have sued over their genetic material before haven’t had much success.”
While laws regarding medical consent have changed since Lacks died, companies still use our genetic material all the time, he said.
“You’ve probably already many times given consent for the secondary use of a bunch of your body materials – when you’ve gone for a blood test, if you’ve ever had a surgery,” he said. “Most of us have. There is a piece of paper somewhere that we’ve signed that indicates that this is the case.” But Attorney Crump, who also represented the family of George Floyd killed in Minneapolis by convicted former policeman Derek Chauvin, is confident.
“Respect the fact that Henrietta Lacks’ life mattered, that Black Lives Matter,” he said during the NPR interview. “This is what we mean by trying to have a racial reckoning in America.”














